The Future of Healthcare Telemedicine Solutions
- Josh Orueta
- December 11, 2020
Updated on January 14, 2022
What Has Led to the Boom in Telemedicine Platforms?
Since the COVID-19 pandemic began, the need for global telemedicine platforms has skyrocketed. Prompted by the public health emergency, the US government introduced new policies and began heavily investing in and funding healthcare telemedicine solutions.
The Federal Communications Commission (FCC) COVID-19 Telehealth Program allocates funds to eligible healthcare providers to promote the use of telemedicine services, and new CMS policies support reimbursement for video visits[¹]. Further, the Families First Coronavirus Response Act[²]ensures that patients are not required to pay for telemedicine consultations related to COVID-19 testing and treatment.
As an emergency measure, the Office for Civil Rights (OCR) at the Department of Health and Human Services permits healthcare providers to use non-HIPAA-compliant video conferencing software for telehealth services during the pandemic[³]. Medical practitioners using these technologies will temporarily not be subject to penalties for non-compliance with HIPAA rules.
Recommended reading: The Rise Of Telehealth Software During COVID-19
Does Telemedicine Software Provide Patients With the Best Care Experience?
As the demand for telehealth has skyrocketed, so has the number of telemedicine companies that provide telehealth consultations with a physician network. MDLive®, for example, connects users with healthcare professionals 24-hours a day, by phone or live video. Insurance companies[⁴]are now partnering with these providers. Although convenient, network telemedicine platforms like MDLive® do not guarantee that a patient will use the same practitioner after a visit. Receiving virtual care from a provider network ignores a foundational component of effective health care: patient-provider relationship building. After all, continuity of care is a fundamental tenet of primary care[⁵].
A recent study published in the journal BMC Family Practice[⁶] explored the positive and negative impacts of using telehealth during the COVID-19 pandemic. Researchers found that physicians were concerned about the potential weakening of therapeutic relationships, limited patient engagement, the lack of psychosocial support, establishing trust and relationships with patients, the depersonalization of practice, and changes in patients’ expectations. The physician respondents also noted that the therapeutic relationship was particularly difficult to establish using telehealth when they had no previous relationship with the patient.
From the patient’s perspective, a 2020 Mayo Clinic®[⁷]study found that patients value the ability to build a clinician-patient relationship through telemedicine. The study also concluded that patients who are satisfied with their telemedicine encounters appreciate the overall user experience, which includes convenience and access.

If a patient’s primary care network has not adopted telemedicine software, the patient may be forced to use outside services. Healthcare organizations need a healthcare telemedicine solution where physicians can conduct virtual visits, thereby retaining existing patients and attracting new ones.
In order to quickly meet the telemedicine needs of patients during this public health emergency, providers have been permitted to use non-HIPAA-compliant solutions such as Apple FaceTime®, Facebook Messenger™, Skype™, WhatsApp®, and Zoom®. Healthcare organizations will not be able to offer telemedicine services in this manner indefinitely; the HIPAA waiver will expire. Implementing a secure HIPAA-compliant telehealth service should be a priority.
Recommended reading: Telehealth vs. Telemedicine
Most Wanted Features of Telemedicine
A telemedicine solution shouldn’t be a giant stretch from a healthcare provider’s normal workflow. Familiarity will help both patients and providers adapt to telemedicine technology.
Features of telemedicine should allow patients to do the following:
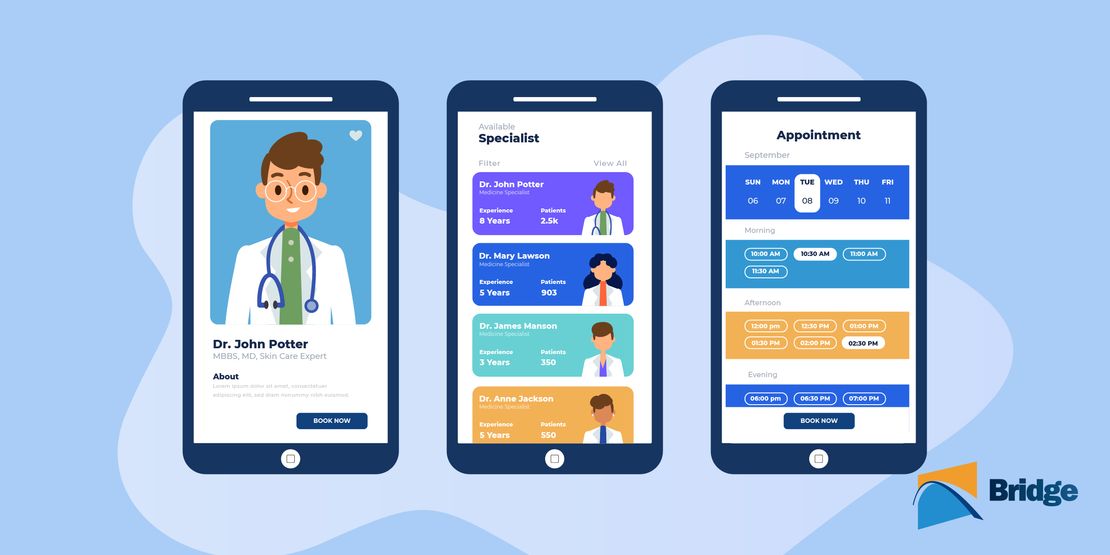
- Self-schedule telemedicine appointments online via a medical scheduling software
- Get a notification to start/join their telemedicine visit
- Receive guidance on what to expect for their first visit, including explaining hardware setup
- Access a virtual waiting room
- Message or chat with staff to troubleshoot audio/video issues
- Interact with providers using videoconferencing or audio, with the option to conference in an interpreter, caregiver, or notetaker if needed
- Share images and files during the telemedicine visit
Features of telemedicine should allow providers to do the following:
- Streamline and maximize the efficiency of the consultation, whereby patients can complete the administrative process and be fully ready in a virtual waiting room before the live face-to-face 5 to 10-minute consultation
- Reduce the burden of travel for both patients and providers, especially patients managing chronic health conditions, while adding the flexibility to extend care beyond normal hours
- Increase their patient base while improving access to rural and underserved populations
- Seamlessly share and store records, test results, prescriptions, and billing information[⁸]
A telemedicine solution should seamlessly integrate with clinics’ Electronic Health Record (EHR), Revenue Cycle Management (RCM), or Practice Management (PM) source systems. Healthcare providers should be able to share data bidirectionally between the source systems and their telemedicine platform.
Healthcare Telemedicine Solutions in 2022 and Beyond
In 2020 and 2021, telemedicine experienced substantial growth, and patients continue to embrace virtual care. As healthcare organizations race to implement healthcare telemedicine solutions, many are wondering if funding, reimbursement, and usage will continue.
Previously, health care providers experienced difficulties in receiving reimbursement for telemedicine services as states charged for telemedicine in different ways. Now, payments for a telemedicine visit are made as easily as an in-person visit. This transition is encouraging to providers who wish to continue to provide telemedicine services to their patients.
When the HIPAA waiver expires, healthcare providers will no longer be able to use non-HIPAA-compliant video communication platforms for consultations, and organizations will need to implement secure, reliable HIPAA-compliant telemedicine software.
Though brought in by a public health emergency, telemedicine is expected to remain a permanent fixture in healthcare.
“Virtual care solutions bring health care to the consumer rather than the consumer to health care,” said Brian Marcotte, President, and CEO of the National Business Group on Health[⁹].
“They continue to gain momentum as employers seek different ways to deliver cost-effective, quality health care while improving access and the consumer experience.”
By leveraging telemedicine as part of a comprehensive patient engagement solution, providers can meet patient demand for the digital solutions they have now come to expect.
DISCLAIMER: All product and company names are trademarks™ or registered® trademarks of their respective holders. Bridge Patient Portal is not affiliated with, nor has it endorsed or sponsored in any way, the service providers mentioned in this article.
- www.cms.gov. (2020). Medicare Telemedicine Health Care Provider Fact Sheet | CMS. [online] Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- Lowey, N.M. (2020). Text – H.R.6201 – 116th Congress (2019-2020): Families First Coronavirus Response Act. [online] www.congress.gov. Available at: https://www.congress.gov/bill/116th-congress/house-bill/6201/text.
- Office for Civil Rights (OCR). (2020). Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. [online] HHS.gov. Available at: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html.
- Japsen, B. (n.d.). Cigna Expands MDLive telemedicine Partnership To Primary Care. [online] Forbes. Available at: https://www.forbes.com/sites/brucejapsen/2020/01/13/cigna-expands-mdlive-telehealth-partnership-to-primary-care/.
- Bergman, D., Bethell, C., Gombojav, N., Hassink, S. and Stange, K.C. (2020). Physical Distancing With Social Connectedness. [online] The Annals of Family Medicine. Available at: https://www.annfammed.org/content/18/3/272#ref-13.
- Breton, M., Sullivan, E.E., Deville-Stoetzel, N., McKinstry, D., DePuccio, M., Sriharan, A., Deslauriers, V., Dong, A. and McAlearney, A.S. (2021). Telehealth challenges during COVID-19 as reported by primary healthcare physicians in Quebec and Massachusetts. [online] BMC Family Practice. Available at: https://bmcfampract.biomedcentral.com/articles/10.1186/s12875-021-01543-4#citeas.
- Elliott, T., Tong, I., Sheridan, A. and Lown, B.A. (2020). Beyond Convenience: Patients’ Perceptions of Physician Interactional Skills and Compassion via Telemedicine. [online] Mayo Clinic Proceedings. Available at: https://www.mcpiqojournal.org/article/S2542-4548(20)30075-8/fulltext.
- C2C. (2021). Telehealth For Providers: What You Need To Know. [online] C2C. Available at: https://www.cms.gov/files/document/telehealth-toolkit-providers.pdf.
- Business Group on Health. (2019). Large Employers Double Down on Efforts to Stem Rising U.S. Health Benefit Costs which are Expected to Top $15,000 per Employee in 2020. [online] Business Group on Health. Available at: https://www.businessgrouphealth.org/who-we-are/newsroom/press-releases/large-employers-double-down-on-efforts-to-stem-rising-us.