The unexpected benefit a patient portal has on your MIPS / MACRA score
- Blake Rodocker
- August 14, 2017

Outdated as of May 2021.
This article is outdated. Please find our updated resource that explains the current MACRA / MIPS / Meaningful Use regulations.
Strategies for MIPS / MACRA attestation, and how patient portals might have a greater impact on your scoring than you might think.
The objective of this article is to provide a detailed explanation of the four categories that make up the Merit-based Incentive Payment System (MIPS) point system that affect an eligible provider’s reimbursement, and how a patient portal helps a provider attest for these four categories. MIPS is one of 2 reimbursement tracks under MACRA. For a primer on MACRA – who qualifies for the program, the reporting/adjustment timeline, the reimbursement/penalty rates, and how MIPS relates to MACRA – please read our earlier post MACRA 101: An explanation by Bridge Patient Portal. So let’s learn about certified MIPS / MACRA patient portals and how they can help.
What are the four categories that makeup MIPS?
MIPS is made up of four performance categories. It represents several previously existing Medicare reporting programs, renovated and rolled into one. Here, we list the MIPS performance categories in order of potential for patient portal impact (highest to lowest):
- Advancing Care Information – Focuses on information exchange and interoperability, replacing the Medicare and Medicaid EHR Incentive Program also known as Meaningful Use (Stages 1 and 2)
- Quality – Measures a provider’s delivery of Quality Care, replacing the Physician Quality Reporting System (PQRS) which expired in 2016, and incorporating the Value-Based Payment Modifier system.
- Improvement Activities – A new category created to measure a provider’s focus on care coordination, beneficiary engagement, and patient safety.
- Cost – Relates to resource use, replacing the Value-Based Payment Modifier. The cost category will be calculated in 2017, but will not be used to determine a provider’s payment adjustment until 2018.
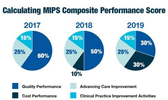
Over the next few years, the weight of each MIPS performance category will change in the calculation of the MIPS composite score – as described in the image below.
The 4 categories of MIPS and how a patient portal can directly or indirectly impact scoring:
1. Advancing Care Information
| Value | Patient Portal Impact (Low, Medium, High) | Ease of Implementation (Easy, Medium, Hard) |
|---|---|---|
| 25% | High | Medium |
ACI is highly dependent on patient portal technology, with about half of its sub-category measures achievable through patient portal features. With the use ofcertified patient portal technology, physicians can accumulate MIPS points with relative ease. Below is a table listing the different measures for the ACI category.
Most everyone is familiar with the recently sunsettedMeaningful Use Stage 2 program, where incentive payments were paid (or overpaid) to providers with patient portals that provided at least 50% of their patients with access to their medical records online, and at least 1 patient per eligible provider was required to view, transmit and download their health summary. Advancing Care Information (ACI) essentially replaces the Meaningful Use program and raises the bar further.
Base Score Advancing Care Information Measures and Scores 2017 Advancing Care Information Transition Measures and Scores Required Measures for 50% Base Score % Points Required Measures for 50% Base Score % Points - Security Risk Analysis
- e-Prescribing
- Provide Patient Access*
- Send a Summary of Care*
- Request/Accept Summary Care*50% - Security Risk Analysis
- e-Prescribing
- Provide Patient Access*
- Health Information Exchange*50%
NOTE: These measures are also included as performance score measures and will allow a clinician to earn a score that contributes to the performance score category (see the list below).
Measures for Performance Score Advancing Care Information Measures and Scores 2017 Advancing Care Information Transition Measures and Scores Measures % Points Measures % Points Provide Patient Access* Up to 10% Provide Patient Access* Up to 20% Send a Summary of Care* Up to 10% Health Information Exchange* Up to 20% Request/Accept Summary Care* Up to 10% View, Download, or Transmit (VDT) Up to 10% Patient Specific Education Up to 10% Patient Specific Education Up to 10% View, Download or Transmit (VDT) Up to 10% Secure Messaging Up to 10% Secure Messaging Up to 10% Medication Reconciliation Up to 10% Patient-Generated Health Data Up to 10% Immunization Registry Reporting Up to 10% Clinical Information Reconciliation Up to 10% Immunization Registry Reporting 0 or 10%
TheAdvancing Care Information Performance Category Fact Sheet provided by CMS provides an excellent detailed explanation on how the ACI category is scored. In summary, providers must demonstrate at least 1 transaction for each of the categories to receive a 50% “Base Score” for the ACI category (NET 12.5% for the entire MIPS program). To score for an additional 50%, the “Performance Score,” providers must demonstrate additional usage in the “Performance” and “Bonus” categories. Scoring for both the “Base Score” and “Performance Score” allows a provider to achieve 100% scoring.
Important Tips and Information
- October 2nd, 2017 is the last possible start date for 2017 MIPS reporting, including the ACI category.
- Data submission to CMS for 2017 reporting begins on January 1, 2018 and ends on March 31, 2018.
- Both 2014 and 2015 Certified technologies can be used for attesting in the 2017 transitional year of MACRA, so long as the technologies support the ACI measures. There are two measure set “options” Advancing Care Information Objectives and Measures or 2017 Advancing Care Information Transition Objectives and Measures, listed above. In 2017, only the latter requires 2015 certified technology. In 2018, however, 2015 certified technology will be required across the board.
- Some clinicians may not have sufficient ACI measures applicable to them. In such scenarios, the ACI performance category will be reweighted to 0 percent and the 25 percent weight originally allocated to ACI will be redistributed to the Quality performance category. This may be the case for clinicians who are hospital-based or qualify for a hardship exemption.
- If the minimum required measures (listed in the table above) for the Base Score are not met, the provider will receive a score of 0 for the entire ACI category.
2. Quality
Value Patient Portal Impact
(Low, Medium, High)Ease of Implementation
(Easy, Medium, Hard)60% 2017
50% 2018
30% 2019Medium Hard
MIPS has created the Quality performance measure category by merging the Physician Quality Reporting System (PQRS) and Value Based Modifier (VBM) programs. While the quality category offers the most value opportunity, it can be the most difficult to report on. The reporting period is the entire year, unlike the 90 day period for the ACI category. In most cases, providers must select 6 quality measures to report on from the many available in thislist.
A well implemented patient portal can have a significant impact on a provider’s Quality performance. Much of the Quality category scoring has to do with improved outcomes that in many cases benefit from an engaged patient population. This can be achieved through patient portal functions like patient reminders (appointment, care plan, Rx refill, etc.), notifications, and patient-provider messaging. A provider will also receive points for delivering Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys, which can be administered electronically. To directly use a patient portal, or Certified EHR Technology (CEHRT), for reporting, the CEHRT must be certified on the measure being reported. Providers can earn additional bonus points by reporting with a CEHRT. The measures must be eligible, and reporting must be done entirely with the CEHRT. The maximum number of CEHRT bonus points is 10% of the maximum score, which would be 6% in 2017 as the value is 60%.
The many different scenarios available to providers for the Quality category further complicate the already complicated scoring system. But essentially, each measure gets a score of 1-10 points (0 points if not reported) compared to historical benchmarks (if available). With a perfect score of 10 in each of six measures, providers receive 60 points, or a full score.
Important Tips and Information
- Most providers must report up to six Quality measures so long as one measure is an outcome measure (or a high priority measure if no outcome measure applies to the provider). Groups of 25 or more providers may use the CMS Web Interface, in which case they will need to report on 14 different measures. CMS plans to increase the number of measures to report on in future years.
- Selecting the right measures is of utmost importance. CMS scores a provider in comparison to other providers (benchmarking), making it is easier to score in the top percentile on some measures compared to others. We recommend seeking guidance from a consulting firm or expert on MIPS in order to identify the best categories for your situation.
- The Quality performance measure category has been sub-categorized into Efficiency, Intermediate Outcome, Outcome, Patient Engagement/Experience, Process and Structure measures.
- In 2017, the Quality score weight has been set to 60% unless the provider has applied for an ACI exclusion. In this case, the 25% ACI category value will be applied to the Quality category, increasing the quality category value to 85%.
- Providers qualifying for one of the specialty measure sets may report fewer than six measures (in some cases), or select six measures from the specialty measure set.
- MIPS essentially adopts the quality measures and reporting methods from the Physician Quality Reporting System and Volume Based Modifier programs. Although there are some changes to the PQRS reporting methods, for the most part the quality reporting methods remain the same.
- Practices must use the latest annual measure update. For instance, for the 2017 performance period, practices must use the eCQM specifications contained in the 2016 annual update, released in April 2016.
3. Improvement Activities
Value Patient Portal Impact
(Low, Medium, High)Ease of Implementation
(Easy, Medium, Hard)15% Medium Easy
The Improvement Activities performance category is significantly simpler than the two aforementioned categories, focusing on care coordination, population health, beneficiary engagement, and patient safety. Providers must select only four measures from thislist of more than 90 options and report on these four measures for a minimum of 90 days.
A well implemented patient portal has a variety of features that can be applied to the Improvement Activities performance category measures. Given the focus of the category on care coordination, patient engagement through a patient portal plays a crucial role. For example, there is a specific, medium-weight activity titled “Engagement of patients through the implementation of improvement in patient portal,” “Proactive management of chronic conditions and prevention care,” and “Engagement of patients, family and caregivers in developing a plan of care,” along with a variety of other activities where a patient portal can directly or indirectly be applied to meet requirements.
The Improvement Activities category has a maximum score of 40, which contributes 15% to the MIPS composite score. Each activity is worth 10 points. Some activities are categorized as “high-weight” (about one fifth of the 90+ activities) whereas the rest are “medium-weight.” High-weight activities are technically worth 20 points, as they hold twice the value of medium-weight activities.
Important Tips and Information
- Physician groups with fewer than 15 participants or in a rural or health professional shortage area can attest by completing up to two (2) activities for a minimum of 90 days, instead of the minimum four.
- CMS allows for submission of data for the Improvement Activities performance category using the qualified registry, EHR, QCDR, CMS Web Interface as attestation data submission mechanisms.
4. Cost
| Value | Patient Portal Impact (Low, Medium, High) | Ease of Implementation (Easy, Medium, Hard) |
|---|---|---|
| 0% 2017 10% 2018 30% 2019 | N/A | N/A |
Various primary care services are used to calculate the total per capita cost measure. Chronic care management (CPT code 99490) is an example of a primary care service that can be facilitated through Chronic Care Management (CCM) Software linked to a patient portal or EHR. Patient portals such as Bridge Patient Portal also have the ability to facilitate annual wellness visits (G0438 and G0439) or welcome to Medicare visits (G0402) through the use of appointment reminders and care plans.
The Cost category, which replaces the Value-Based Payment Modifier, requires no reporting. All its measures are derived from Medicare claims data, therefore participation does not require data submission. Furthermore, the Cost category is not included in the 2017 payment modifier.
Conclusion
The trend we are seeing with CMS programs, like MACRA and its previous iterations, is a greater emphasis on patient engagement and quality of care. It’s hard to imagine a future where patients aren’t able to access their information, manage their care plans and communicate with provider online. We strongly believe that putting a strong emphasis on online patient engagement, leveraging solutions like Bridge Patient Portal, not only has a direct impact on MACRA scoring, but paves the way for a smooth transition from fee-for-service to fee-for-value reimbursement models.
MIPS Patient Portal
Bridge Patient Portal is a MIPS patient portal with a 2015 Edition ONC Health IT Certification. Bridge Patient Portal v2.0 has been certified by SLI, an Office of the National Coordinator-Authorized Certification Body (ONC-ACB) in accordance with the certification criteria adopted by the Secretary of Health and Human Services (HHS). The portal helps increase patient engagement while helping provider groups meet requirements for MIPS/MACRA.