- Josh Orueta
- July 30, 2021
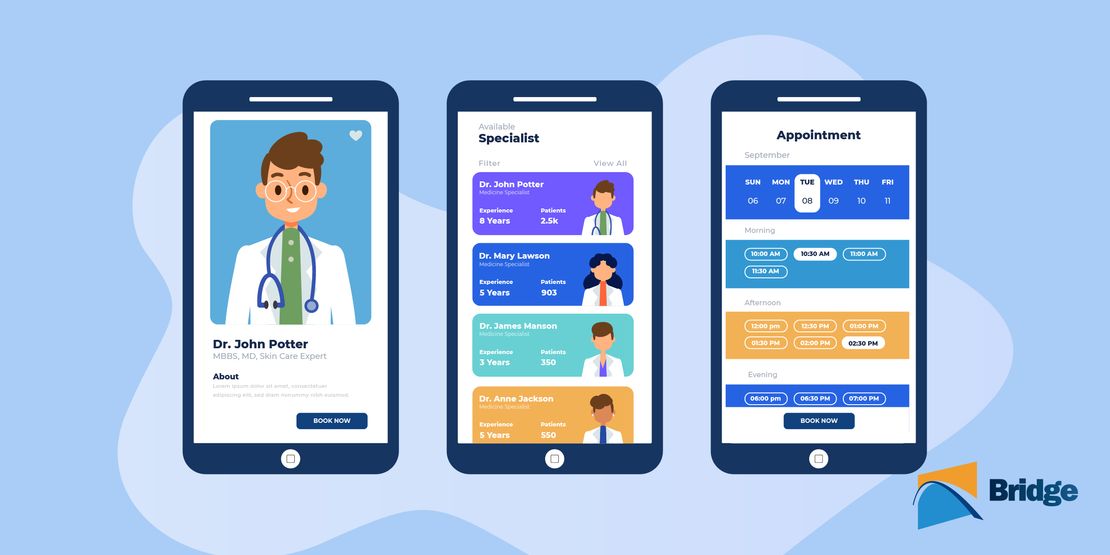
Why Your Organization Needs a Healthcare API

Healthcare is currently undergoing a massive phase of digitalization as it strives to shape its structures for the modern world, while also giving patients better access to both their practices and their health data, as mandated by the 2016 Interoperability and Cures Act[¹]. In 2020, nearly 50% of healthcare providers…Read more